Maternity Care Moves To ERs As Hospitals Face Financial Pressure
More women are delivering babies in emergency rooms as maternity wards disappear. In Los Angeles County, about 14% more women sought birthing care in ERs in 2023 than in 2016, even as overall births fell 26%, according to new reporting by Type Investigations and The Guardian. Between 2016 and 2023, more than 26,500 people — roughly 64% Latino — delivered in ERs.
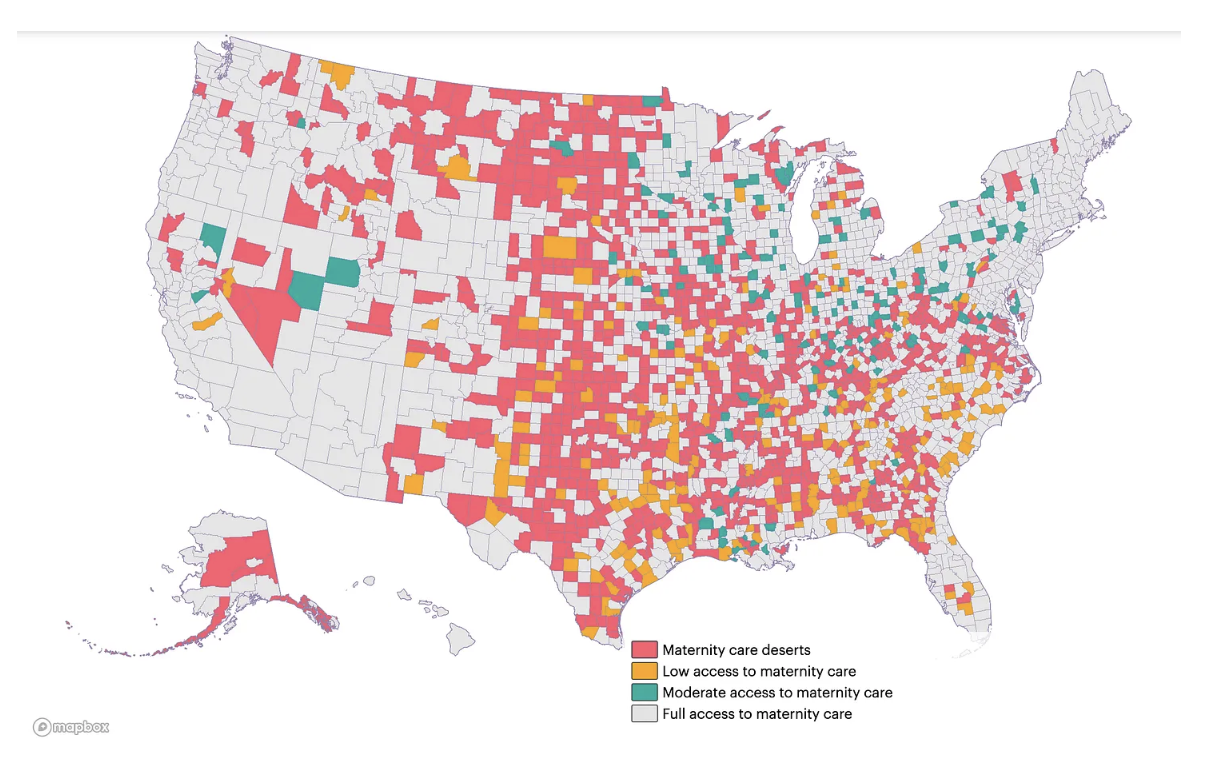
One major driver: maternity ward closures. L.A. County has lost at least five since 2023 and 16 since 2014, leaving many patients with no other option. Nationwide, more than 35% of U.S. counties are maternity care deserts — meaning there are no hospitals offering obstetric services or birth centers, and no obstetricians, gynecologists, or certified nurse midwives.
BIGGER PICTURE
These deserts are mostly concentrated in rural areas across the South and Midwest, but cities are increasingly being affected too. More than 500 hospitals dropped obstetric services from 2010–2022, according to research published in JAMA. And ERs can’t turn patients away in the case of an emergency.
Costs are partially to blame for the closures.
Maternity wards require 24/7 staffing and are comparatively expensive to operate. Hospital administrators also point to declining birth rates, rising costs, and labor shortages as reasons for the closures.
Funding for hospitals is on the line. President Trump’s tax and spending bill, passed this summer, reduces federal Medicaid — the program that pays for 41% of all U.S. births.
The U.S. has the highest rate of maternal deaths of any high-income nation. ER doctors are trained to handle a wide range of emergencies — not to provide comprehensive prenatal, labor, and postpartum care.